Thyroid Specialist Melbourne
For patients or GP’s searching for a thyroid specialist or thyroid surgeon in Melbourne, our team of ENT specialists is here to help. Our thyroid surgeon Dr Sam Flatman has completed a further sub-specialisation in advanced Head & Neck surgical oncology, thyroid and parathyroid surgery. On this page we will help you understand more about thyroid nodules, thyroid cancer, surgeon-performed ultrasound, goiter, thyroid surgery and thyroidectomy.
The role of the thyroid
The thyroid is a soft, butterfly shaped gland situated in the base of your neck in front of the trachea or ‘windpipe’. It has two rounded sections called lobes that are joined by a thin section called the isthmus. The thyroid releases hormones into the body that help regulate body functions relating to metabolism, growth and development.
Thyroid Nodules and Thyroid Cancer
Thyroid nodules are solid or fluid-filled lumps that form within your thyroid and are extremely common. While thyroid nodules may be found during a physical examination of the neck, many are found incidentally through other investigations such as ultrasound, CT, MRI and PET scans.
Approximately 5% of all thyroid nodules are cancer. Most of these will be small papillary thyroid cancers where the survival rate is very high at 98-99%. Thyroid nodules should be approached at least initially with these facts in mind.
Increase in diagnosis of thyroid cancer
There has been an exponential increase in the diagnosis of thyroid cancer in high-income countries. This is due to patients having easy access to high frequency ultrasound, which is being performed often for unrelated conditions. Around 50% of thyroid cancers are estimated to be micro-papillary thyroid cancers that are less than 1 cm in size.
Typically these types of cancers would largely have gone undiagnosed and not have caused a clinical problem. Autopsy studies have shown that in some countries up to 30% of people have these small thyroid cancers that were never identified. Importantly, with this exponential increase in the diagnosis of thyroid cancer, the mortality rate from thyroid cancer (which is very low) has remained the same.
Thyroid nodule investigation
Facts such as these have tempered the investigation of thyroid nodules. Currently, the movement is toward more conservative investigation of thyroid nodules and more conservative thyroid surgery. For example, nodules less than 1cm in size are not recommended for investigation with ultrasound-guided fine-needle aspiration (US-FNA).
Furthermore, there is a movement toward ultrasound surveillance for confirmed, low-risk, small papillary thyroid cancers in properly selected patients who do not undergo any surgery at all. This is called active surveillance, for which there is now long-term evidence from trials in Japan and the USA, for example. There is a shift to streamline the patient process, limit over-treatment, reduce error and reduce patient morbidity.
The gold standard for the management and work up of thyroid nodules is set out in the ATA (American Thyroid Association) Guidelines. Our surgeons are up to date with these guidelines and manage patients accordingly.
Surgeon-performed ultrasound for thyroid nodules
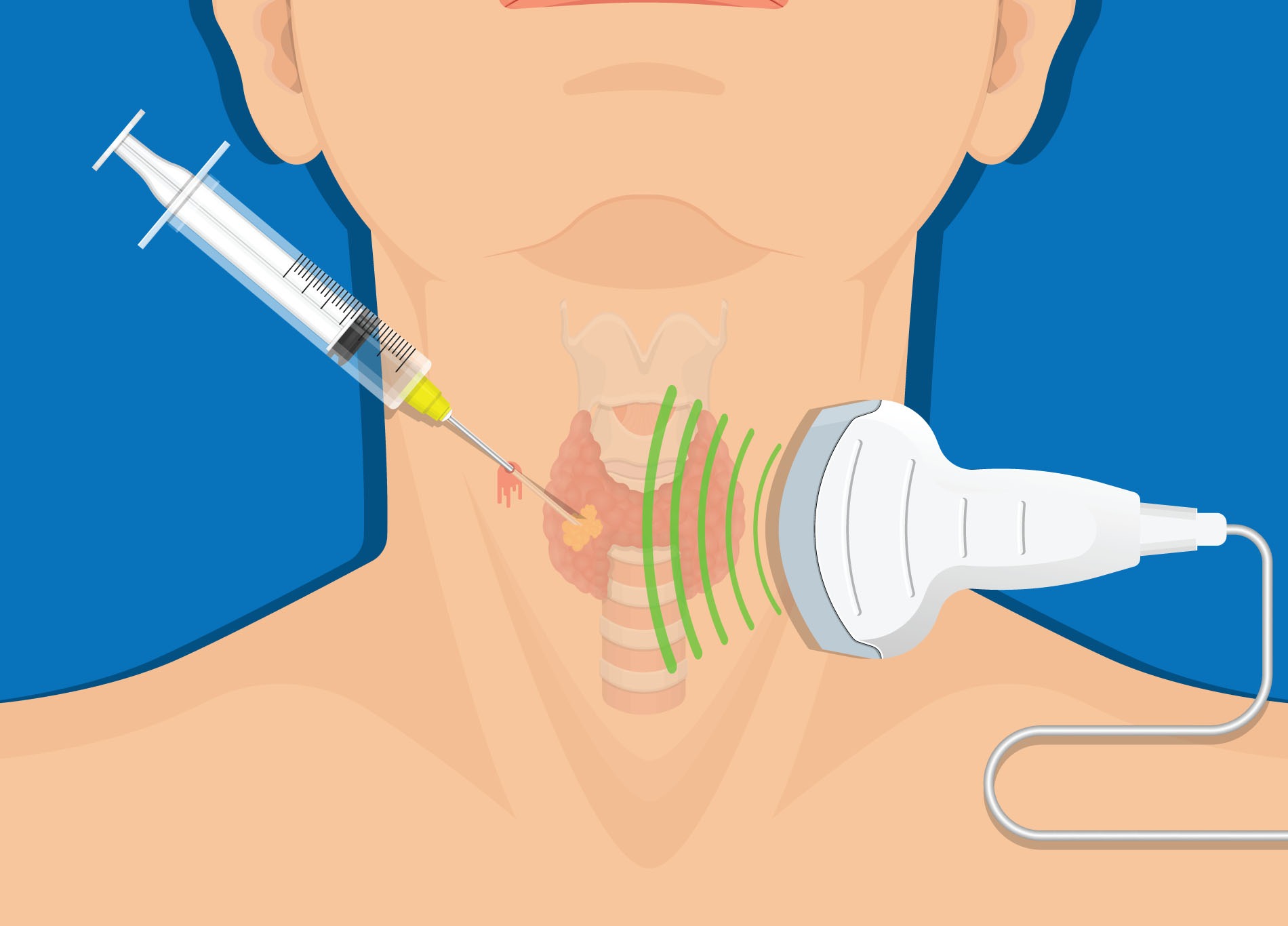
The workup of thyroid nodules to rule out cancer includes ultrasound and US-FNA. Surgeon-performed ultrasound (where the specialist surgeon performs their own dedicated ultrasound on the patient in the office) has been shown to change the surgical management in nearly half of patients with thyroid cancer and is performed internationally by thyroid experts.
It also allows the surgeon to perform immediate US-FNA on the same day as the consultation, and has been shown to streamline diagnosis while decreasing the number of appointments, travel, costs and stress for patients.
Finally, evidence has shown that patients have better outcomes and less complications when treated by high-volume thyroid surgeons.
Goiter – enlarged thyroid glands
A thyroid goiter is an enlarged thyroid gland. This can result from different causes, including iodine deficiency, autoimmune thyroid disease, genetic conditions and thyroid nodules. Most goiters are actually benign.
In many instances surgery is not indicated and patients do not need to have an operation unless the enlarged gland is causing a problem. Indications for surgery include swallowing or breathing problems (resulting from pressure from the enlarged goiter) or cosmetic and aesthetic issues related to its size. Sometimes, it can be associated with cancer. Otherwise, goiters can be safely observed until they cause symptoms, if they ever do at all.
Thyroid surgery
Thyroid surgery can include the surgical removal of part or all of your thyroid gland. It may be performed to treat thyroid disorders such as overactive thyroid/hyperthyroidism, cancerous nodules and goiter.
Total thyroidectomy refers to the removal of the entire thyroid gland. Hemithyroidectomy is the removal of half the thyroid gland.
Parathyroidectomy is a surgical procedure where a parathyroid adenoma is removed and is often performed on patients with primary hyperparathyroidism.
Goiter surgery
Most goiters can be successfully removed with a standard thyroid operation, involving a limited small incision in the lower neck. Very rarely, some goiters are so large they extend below the neck into the chest. These ‘retrosternal’ goiters can often still be removed via the neck, however sometimes a mini-sternotomy may be required. This technique, as compared to conventional ‘full’ sternotomy, involves a smaller incision and has been associated with decreased pain, faster recovery and shorter hospital stay.
Our Thyroid Surgeon – Dr Sam Flatman
Dr Sam Flatman is an Otolaryngologist Head & Neck Surgeon and a Fellow of the Royal Australasian College of Surgeons. He has completed a further sub-specialisation in advanced Head & Neck surgical oncology, thyroid and parathyroid surgery in North America. He is also the senior surgeon treating advanced and metastatic thyroid cancer at Peter MacCallum Cancer Centre and has presented and published in this field both nationally and internationally.
Dr Flatman has formal training and accreditation in Head & Neck ultrasound, issued by the American College of Surgeons and the American Head and Neck Society. He is one of only a few surgeons in Australia who performs their own ultrasounds and ultrasound-guided fine-needle biopsies as part of the workup of thyroid nodules, benign neck lumps and cancers of the head and neck.
Sources: https://www.mja.com.au/journal/2004/180/5/6-thyroid-nodules-and-thyroid-cancer